Inflammation has been found to be a key underlying process in the development of a huge number of chronic diseases. These range from Alzheimer’s disease, to cardiovascular disease, to autoimmune conditions, asthma and eczema, the list goes on. In this article, I will try to explain what inflammation is fundamentally, why too much is bad and some of the ways you can reduce the burden of inflammation on your health.
What is inflammation?
To start, we need to define what inflammation is. Inflammation is a necessary biological process that has been preserved through evolution because it is critical to our survival. It is the cellular and biochemical process of how our bodies (largely our immune system) responds to injury (or the threat of it) and eventually heal. The injury can be traumatic, infective, toxic, or can come in many other shapes and sizes.
When inflammation occurs in response to injury to cells, it is the first step towards healing in that cell or tissue. When inflammation occurs before any actual damage has occurred, it is usually in response to a perceived external threat. One example of this is the foreign bacteria that has entered your body uninvited and that could make you very sick.
Both are situations where inflammation is desirable. However, like with almost everything in the body (and life), balance is everything. An inflammatory response in the body can cause a problem if for example it is:
- Too strong – for example in patients who become very unwell with COVID-19
- Persistent for too long – for example chronic eczema or asthma, causing lasting damage to your cells and tissues.
- Inappropriately activated – in response to a non-harmful trigger, e.g. the body reacting against its own tissues in conditions like rheumatoid arthritis or inflammatory bowel disease.
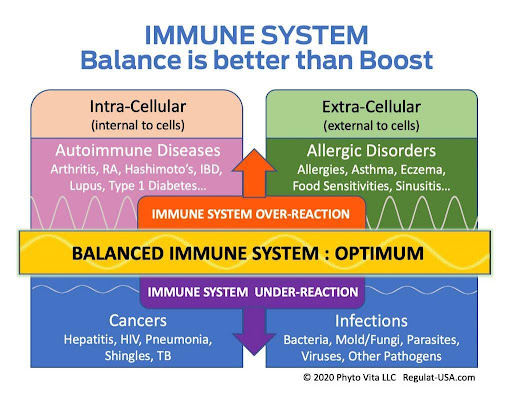
Promoting balance
The inflammatory state of our bodies is always in fine balance. The immune system works in a way that means when inflammation is present, anti-inflammatory process that will halt the march of inflammation are simultaneously activated. Think of inflammation as a fire which our immune system lights and regulates. How this fire burns and for how long is hugely affected by many modifiable lifestyle factors.
Such factors include:
- The balance of dietary fatty acids (omega-3 vs omega-6)
- Our gut microbiome
- Phytonutrient and antioxidant intake
- How much sugar and ultra processed food we consume
- Stress levels
- The amount of fat (adipose) stores we have
- Environmental toxin exposures
It is important to highlight that five of the eight points above are factors relating to your gut or nutrition. This is no coincidence. The inside of your gut is your biggest interface with the outside world and is the source of the biggest source of signals to your immune system, and physiology.
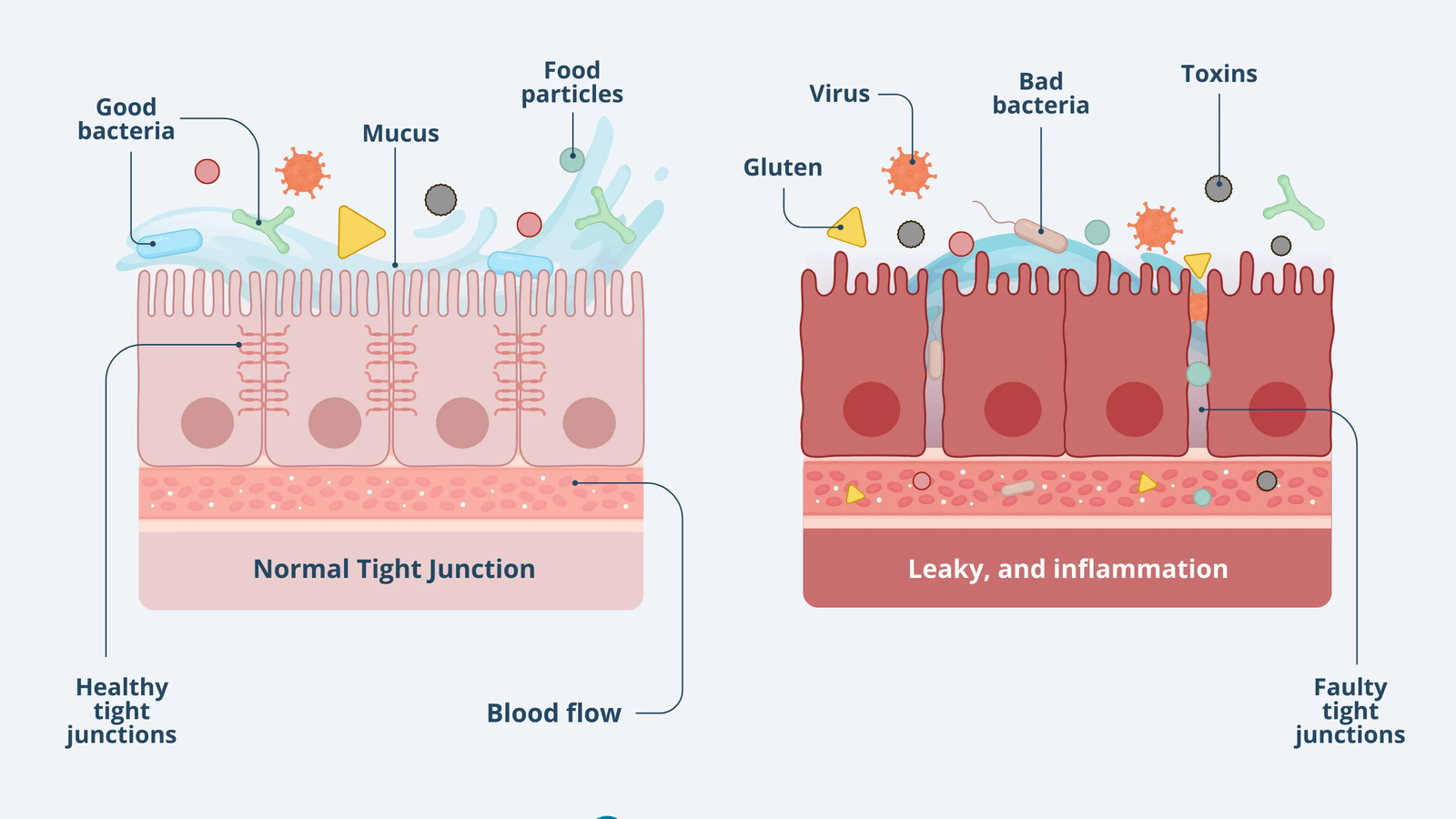
The health of your gut barrier
Localised inflammation due to imbalances or insults to the gut lining from any of the above can trigger a cascade of events. Local inflammation causes damage to the integrity of the gut barrier. This means that a greater number of immunogenic (immune system triggering) particles from inside your gut can move into your blood stream with greater ease. This in turn can trigger a more widespread immune response in the whole body.
This process is called the development of a “leaky gut”. A leaky gut can result in a number of symptoms as the immune system reacts. These include joint and muscle aches, IBS, headaches, fatigue, brain fog, chronic runny nose, to name a few. It is also a common initiating event in otherwise unexplained chronic inflammatory or autoimmune conditions like eczema or inflammatory bowel disease.
It is therefore crucial to maintain a healthy gut barrier function in order to reduce the risk of developing so many chronic conditions.
Heal thy gut
General dietary advice I give to all my patients to optimise their gut health are:
- Have at least 9 different plants a day (daily diversity)
- Consume at least 30 different types of plants throughout the week (long term diversity)
- Eat the rainbow – the colours represent power phytonutrients with anti-inflammatory properties
- Get plenty of healthy unsaturated fats, in particular omega 3s – whether through food sources or supplements
- Avoid ultra processed foods like the plague!
The Agami Approach to Inflammation
At Agami Health, we are able to fully assess for various nutritional and biochemical biomarkers linked to chronic inflammation, as well as assess your gut as a potential trigger or driver of ongoing inflammation due to a leaky gut. We go above and beyond standard medical tests for inflammation which usually just include biomarkers like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR).
Our comprehensive testing allows us to create a tailored treatment plan to treat chronic inflammation. We use personalised nutrition plans as well as supplements and other treatments to restore balance to your gut and reduce your inflammatory burden. We often also advise on strategies such as time restricted eating or intermittent fasting to reduce the burden of inflammation from the gut.
Contact us at Agami Health to find out how we can assess your physiology at a deeper level and optimise your health.