Biological Ageing Clocks – A Critical Perspective from a Longevity Physician
Biological age versus chronological age
Why scientists created ageing clocks
Biological Ageing Clocks: What Are They Really Measuring?
What a younger score really means
Horvath Clocks: The Origin Story
TruDiagnostic and Telomere Length Estimation
GlycanAge: A Different Approach, Different Limitations
Comparing GlycanAge with other tests
What research tells us about reliability
Why this matters for your health
Phenotypic Clocks: A Step Forward, But Are They Useful?
Summary of Modern Clocks and Their Limitations
The Marketing Hype Around Biological Age Clocks
Ethical concerns in the new era
Alternatives and Actionable Approaches
Taking Charge of Your Biological Age
In Summary
Biological ageing clocks claim to estimate how old your body appears using various different techniques such as DNA methylation, glycans and blood biomarkers. They are valuable research tools but remain experimental, often reflecting dysfunction rather than ageing itself. Despite bold marketing, current models lack reliability and utility for individual care. The most effective way to extend healthspan is still through validated markers such as cardiovascular, metabolic, hormonal and inflammatory measures, supported by lifestyle foundations. At Agami Health, we focus on turning robust science into personalised strategies that deliver meaningful and lasting results.
Key Insights
- Chronological age is not the same as biological age. The latter reflects changes in health and resilience, but current clocks capture associations, not causes, of ageing.
- Horvath’s original clock was groundbreaking but highlights volatility in DNA methylation as a measure of ageing.
- TruDiagnostic’s telomere estimates and GlycanAge’s glycan profiling are influenced by short-term stressors and lack external validation.
- PhenoAge combines blood markers and methylation data, making it stronger for population studies but still too blunt for individual care.
- All modern clocks face the same issue: oversimplifying physiology into a single metric, which may be misleading without context.
- Marketing hype often promises to “reverse your age”, but there is no evidence that modifying clock scores translates into longer lifespan.
- Ethical concerns are emerging around AI-driven models and the psychological or financial consequences of being labelled “older” than your years.
- What matters now: Cardiovascular, metabolic, hormonal and inflammatory markers give actionable insight into healthspan. These remain the foundation of longevity medicine at Agami Health.
Biological age versus chronological age
The creation of the very term “biological age” is rooted in the idea that the human body can age at least partially independent of the passage of time, or what we call your chronological age. Detaching our biology from the physical concept of the dimension of time seems very exciting and alluring. This idea may well have some truth in it, but the current challenge lies in defining ageing itself.
What is age itself if not a measure of time? We still do not know the true biological basis of the process of ageing. There are diseases that we see, dysfunction that develops and molecular patterns that emerge with the passage of time, sometimes called the hallmarks of ageing. There is no telling however whether these are downstream consequences of the ageing process, accelerators of ageing or the primary components of the ageing process itself.
A biological ageing clock is a scientific model that claims to estimate how you are ageing by analysing molecular and clinical signals. Unlike chronological age, which simply measures the passage of time, biological age is often linked more closely to healthspan and the risk of age-related disease.
Why scientists created ageing clocks
Biological ageing clocks have been created using various techniques and technologies with the claim that they somehow quantify this underlying ageing process. Different biological ageing clocks use different methods. Some look at DNA methylation, others glycan profiles or other biomarkers to try and capture some facet of what they believe to be the ageing process. Even if they provide a more precise estimate than chronological age, what does this mean in practice? Does a score 20 years “younger” imply an organ functions like that of someone two decades your junior, or that you will live 20 years longer? Evidence suggests not.
Biological clocks mostly measure molecular patterns associated with dysfunction that appear more often as people grow older chronologically. In this sense, epigenetic clocks may be defining age in terms of dysfunction rather than some internal biological time. This distinction matters, because much of the discussion around biological ageing clocks centres on what they are actually quantifying. Are they revealing the essence of ageing, or simply patterns of dysfunction that accompany it? To answer that, we need to look more closely at what these clocks measure in practice.
For a full longevity overview, see our guide on how Agami Health approaches ageing and healthspan.
Biological Ageing Clocks: What Are They Really Measuring?

Most biological ageing clocks are based on Steve Horvath’s work on DNA methylation patterns, giving rise to what we now know as Horvath clocks. Methylation clocks work by detecting tiny chemical tags added to DNA—methyl groups—that regulate gene expression. These patterns fluctuate with time and exposure to environmental factors. Epigenetic data from thousands of CpG sites, analysed with regression models to predict chronological age. The result is a “biological age” number that may be younger or older than your actual age. This figure reflects correlations with disease risk and mortality, not a direct measurement of the ageing process.
What a younger score really means
A “younger” biological age does not necessarily mean you function like someone decades younger, nor that you will live longer than your peers. What these clocks actually capture are molecular or physiological patterns that correlate with age-related dysfunction. They track footprints of change, not the underlying biology of ageing itself.
Why these models are limited
Epigenetic clocks define biological age as the chronological age that best matches your DNA methylation profile when tested. Other clocks use composites of blood or clinical biomarkers of dysfunctional health, which may mislead users into believing they represent ageing. The best way to understand these limitations is to look at where the field began. The first widely recognised epigenetic model was the Horvath clock, which continues to influence nearly all biological age research today.
Horvath Clocks: The Origin Story
The original Horvath clock, created by Steve Horvath, analysed methylation at 353 CpG sites across multiple tissues to estimate biological age. It showed a strong statistical correlation with chronological age in large datasets, yet its ability to predict health outcomes varies between cohorts. This landmark model set the stage for later clocks, including GrimAge, PhenoAge, and DunedinPACE.
The challenge of volatility
A major limitation is that DNA methylation patterns are dynamic. They can shift in response to stress, diet, sleep, or illness, making them unstable markers of “biological age” that surely must not be so volatile. Age is generally thought of as a steady progression, not a number that fluctuates week to week. A tool that suggests you are 40 one day, 30 the next, and 60 soon after risks undermining its own credibility as a measure of ageing. This volatility has prompted researchers and companies to search for alternative signals of ageing. One of the most frequently marketed has been telomere length, often included in consumer reports such as those from TruDiagnostic.
TruDiagnostic and Telomere Length Estimation
Telomere length varies between tissues and even between neighbouring cells. It is influenced by oxidative stress, lifestyle, and illness, which makes single-point measurements unreliable. Although commercial tests promote telomere length as an ageing marker, current evidence suggests it is better interpreted at a population level than in individuals.
One of the better-known consumer offerings in the longevity space is TruDiagnostic, which adds in a second variable as part of its biological age estimate – telomere length. Crucially though, they do not actually measure telomere length. They provide telomere length estimation using a correlation between certain methylation patterns and telomere length. They do not share the methodology and there is no publicly available information as to the validity of this estimation.
Now this may well be a legitimate way of estimating telomere length, but until they provide more transparency around their methods and data, it limits the ability to trust this estimate with meaningful certainty.
Hypothetically even if this test did measure telomere length, here are some further issues to consider:
- High Variability Between Cells and Tissues: Telomere length is not uniform across different cell types in the body. A blood sample, which is what TruDiagnostic typically measures, may not accurately reflect the telomere status of other tissues, such as heart, liver, or brain.
- Dynamic and Context-Dependent: Telomere length can fluctuate over short periods due to acute stress, infection, or even methodological noise in laboratory processing. Single measurements may therefore be misleading.
- Limited Predictive Power: While short telomeres are correlated with disease risk, they are not a deterministic marker. Many people with relatively short telomeres live long, healthy lives, while some with long telomeres experience age-related disease.
- Measurement Methodology: TruDiagnostic uses PCR-based or next-generation sequencing methods to estimate average telomere length. Each method has technical limitations, including sensitivity to DNA quality and amplification bias, which can lead to variability in results.
In summary, while TruDiagnostic telomere testing provides an interesting snapshot, it cannot reliably serve as a precise measure of biological age, nor can it predict functional health or lifespan with certainty.
GlycanAge: A Different Approach, Different Limitations
After telomere-based models, another test that has gained attention is GlycanAge, which focuses on a different process known as glycosylation – the attaching of sugars to other molecules. Glycosylation patterns do shift with age and inflammation, so in theory they can suggest whether someone is ageing faster or slower. In practice, however, they are strongly influenced by short-term immune and metabolic changes, limiting their value for long-term age prediction.
Key limitations of GlycanAge
- Influenced by inflammation and environment: Glycan profiles are sensitive to diet, infection, stress and other exposures. A temporary illness can make your glycan age appear much “older” without reflecting lasting biological change.
- Correlation, not causation: Glycans correlate with chronological age and some disease risks, but there is no evidence they cause ageing. They act as markers of dysfunction, not mechanisms.
- Limited actionable insight: Even if the test reports an “older” biological age, the recommendations are still the same as for general longevity: exercise, balanced nutrition, quality sleep and stress management.
- Cost and accessibility: Tests can be expensive, and the results require careful interpretation by a physician who can integrate them with broader biomarker data.
Comparing GlycanAge with other tests
Unlike telomere-based tools such as TruDiagnostic, GlycanAge is more reflective of immune stress than structural cellular ageing. Inflammation is a recognised hallmark of ageing, but its role is complex, and we already have validated inflammatory markers such as hs-CRP, TNF-alpha, IL-6 and more specific measures like LP-PLA2. These established tests provide clearer, more actionable insights.
What research tells us about reliability
An experiment led by Dr Matt Kaeberlein highlights how fragile these consumer tests can be. He repeated four biological age tests in close succession and found:
- No correlation between different platforms that claimed to measure the same thing.
- Significant variation even in duplicate samples run on the same platform.
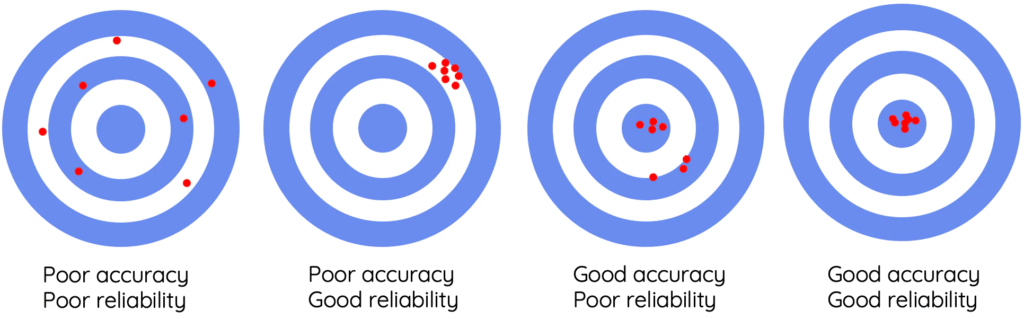
This raises fundamental questions about accuracy, reliability and validity. A weighing scale analogy helps:
- Accuracy: If you weigh 50kg, how close to 50kg does the scale read?
- Reliability: If you weigh 50kg, how similar are repeated readings?
- Validity: If what you actually want to know is waist circumference, is body weight an appropriate surrogate of that metric?
The graphic below shows another visualisation of the concepts of accuracy and reliability.
Why this matters for your health
The science behind these clocks is still at an early stage. They are marketed well and can be fun as a talking point, but in their current form they offer little meaningful insight for healthspan. At Agami Health, we believe biological age testing should not be treated as a badge of honour or shame, but as a reminder that validated biomarkers and personalised strategies remain the foundation for improving longevity.
Phenotypic Clocks: A Step Forward, But Are They Useful?
After glycan and telomere models, researchers sought to improve ageing clocks by combining epigenetic data with standard clinical biomarkers such as CRP and glucose. The idea was to produce a score that predicts disease risk of disease more reliably than clocks based on methylation alone. PhenoAge, developed by Morgan Levine, is the most widely cited example.
How PhenoAge works
PhenoAge combines nine routine blood biomarkers with 513 CpG methylation sites. Together, these inputs generate a composite estimate of biological age that aims to reflect systemic health and mortality risk, rather than simply track chronological time. One advantage is that many of the incorporated biomarkers are already standardised and clinically meaningful.
Strengths and limitations
While PhenoAge outperforms earlier clocks in predicting mortality, it still reduces highly complex physiology into a single score. This makes it more useful for population studies than for guiding personalised treatment. In practice, clinicians still need to break down the score into its underlying systems: cardiovascular, metabolic, immune and hormonal. Only then can the data inform targeted longevity interventions.
The clinical reality
So the key question remains: does collapsing diverse physiology into a single number add value, or does it obscure important details? In the clinic, the latter often proves true. For meaningful care, we must examine each system individually, understand where dysfunction lies and intervene accordingly.
At Agami Health, our philosophy is clear. Composite scores may have research value, but individualised assessment of systems matters more. Human biology is complex, and reducing it to one number risks oversimplification. As Einstein put it: make things as simple as possible, but not simpler.
Summary of Modern Clocks and Their Limitations
Across the consumer space, several biological ageing clocks have gained attention. Each uses a different signal, but all share similar limitations when it comes to clinical application.
| Clock/Test | Primary signal | Strengths | Limitations |
| Horvath (clock) | DNA methylation at 353 CpG sites | First multi-tissue epigenetic clock; strong correlation with chronological age | High volatility; limited predictive power for individuals |
| GrimAge (clock) | DNA methylation patterns linked to mortality risk | Correlates with lifespan and smoking history | Algorithmic complexity; limited actionable insight |
| DunedinPACE (clock) | Epigenetic methylation rate of change | Captures the pace of ageing rather than age itself | Requires longitudinal data; variability remains high |
| PhenoAge (clock) | Combination of 9 clinical biomarkers + 513 CpG sites | Stronger predictor of mortality than earlier clocks | Collapses diverse systems into a single score; requires decomposition for action |
| TruDiagnostic (test) | DNA methylation plus estimated telomere length | Consumer-facing; broad commercial adoption | Method not fully transparent; telomere estimates unvalidated |
| GlycanAge (test) | IgG glycosylation patterns | Reflects immune status and inflammation | Sensitive to short-term changes in health, diet, and stress; limited longevity insight |
What this tells us
Despite different methodologies, these clocks all face the same problem: they simplify complex biology into a single number. This may have research value, but it offers limited help for someone who wants to extend healthspan today. At Agami Health, we believe the priority is validated, actionable biomarkers that guide personalised interventions rather than consumer tests that can mislead.
The Marketing Hype Around Biological Age Clocks
Following the rise of clocks such as Horvath, GrimAge and GlycanAge, consumer companies have promoted them as breakthrough tools for longevity. Marketing often promises to “turn back your biological clock” or “reveal your true age”.
The problem is that most of these claims are not evidence-based. Few consumer tests are supported by peer-reviewed validation, and there is little proof that tracking your biological age improves health outcomes. Marketing materials frequently blur the line between correlation and causation: just because a molecular signature changes with age does not mean that modifying it will slow ageing or extend lifespan.
This creates a predictable cycle. People buy tests expecting actionable advice, receive a single number with little context, and are left frustrated or misled. Without clear guidelines for interpretation, clocks risk becoming novelties rather than meaningful clinical tools.
Ethical concerns in the new era
As artificial intelligence and big data biobanks are used to develop the next generation of ageing clocks, ethical questions become increasingly important. How might biological age data influence insurance, employment, or access to healthcare? What is the psychological burden of being told you are biologically “older” than expected? These are unresolved questions that science alone cannot answer.
Hype versus reality
This is not to dismiss the potential of ageing clocks entirely. They are exciting research tools that may eventually help us understand the biology of ageing. Yet the current consumer offerings are inconsistent, largely unvalidated and often oversold.
At Agami Health, we believe the most valuable tools today remain those with clear evidence, strong clinical relevance and actionable guidance. Biological clocks may one day complement validated biomarkers, but for now they should be regarded as experimental rather than definitive.
Alternatives and Actionable Approaches
If biological ageing clocks are not ready for routine use, what should we rely on instead? In longevity medicine, the focus is on robust, validated markers that translate into personalised interventions:
- Cardiovascular health: Blood pressure, coronary artery calcium scoring, arterial stiffness, lipoprotein profiles, inflammation markers
- Metabolic function: HbA1c, fasting insulin, and glucose variability.
- Hormonal balance: Testosterone, oestrogen, thyroid hormones, cortisol rhythms.
- Inflammation and oxidative stress: hs-CRP, cytokine panels, glutathione, LP-PLA2.
- Lifestyle and nutrition: Sleep quality, physical activity, diet, and stress resilience.
These markers provide both diagnostic clarity and practical direction. They allow clinicians to identify risks early, intervene meaningfully, and monitor the impact of lifestyle or medical strategies on lifespan and healthspan.
As a leading longevity clinic, this is where we focus our work: shifting attention away from abstract numbers towards actionable, personalised strategies that make a real difference.
Taking Charge of Your Biological Age
Biological ageing clocks are promising research tools, but for now they remain experimental. Their appeal lies in simplicity, yet human biology is complex and cannot be captured by a single number.
For individuals who want to extend healthspan, the most effective path is still clear: optimise cardiovascular, metabolic, hormonal and inflammatory markers with guidance from a trained physician. Lifestyle foundations such as exercise, nutrition, restorative sleep and stress management remain the proven cornerstones of longevity medicine.
Our focus at Agami Health is on robust, evidence-based assessments and personalised strategies that make measurable differences to long-term wellbeing. Biological clocks may dominate headlines, but the science of healthy ageing is built on validated markers and actionable interventions, not marketing hype.
If you are ready to take charge of your biological age in a meaningful way, explore Your Longevity Journey with Agami Health.