In the world of longevity medicine, we often talk about the “hallmarks of ageing”—those cellular glitches that accumulate over time. But for approximately half the population, there is a specific biological inflection point that feels less like a slow accumulation and more like a chaotic software update: perimenopause.
At Agami, we view perimenopause not just as a series of inconvenient symptoms to be “managed,” but as a critical window of opportunity to protect your future self.
What is Perimenopause, Really?
While the clinical definition of menopause is reaching the 12-month milestone without a period, perimenopause is the “prequel”—a transition that can last anywhere from months to a decade.
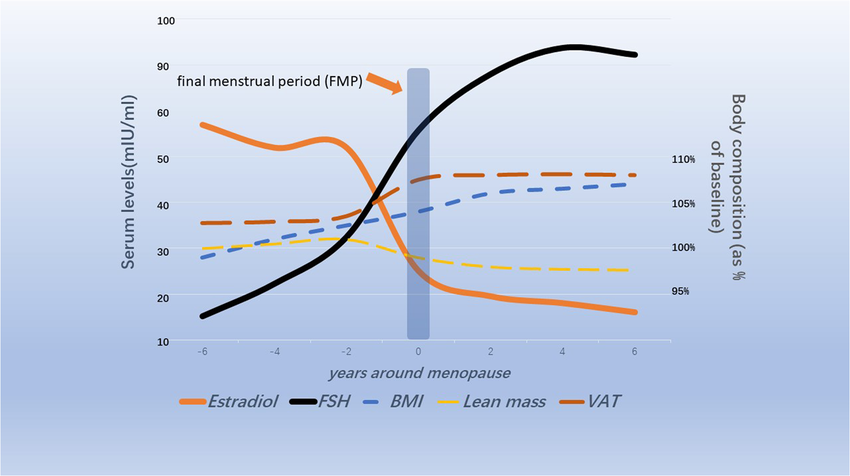
Biologically, it’s a state of “chaostat.” Your ovaries aren’t just turning off; they are sputtering. The most prominent sign of this is a rising Follicle Stimulating Hormone (FSH). Think of your pituitary gland as an over-caffeinated middle manager; when the ovaries stop responding to normal signals, the pituitary starts “shouting” (ramping up FSH) to demand oestrogen production.

But this transition isn’t just about periods. It is a systemic biochemical shift that impacts everything from your neurons to your mitochondria. Fluctuations result in the “classic” hot flushes and brain fog, but can also manifest as joint pain, as the anti-inflammatory “shield” of oestrogen begins to thin.
The Progesterone “Brake Pedal” and the Oestrogen Rollercoaster
The first hormone to typically take a dive is progesterone. Progesterone is your body’s natural valium. It is metabolized into a neurosteroid called allopregnanolone, which plugs into the GABA-A receptors in your brain—the same receptors targeted by anti-anxiety medications.
When you lose progesterone, you lose your biological “brake pedal,” leading to the hallmark perimenopausal triad: anxiety, irritability, and that dreaded “3:00 AM insomnia.”

Oestrogen, meanwhile, doesn’t just decline; it fluctuates wildly. One day you’re at peak levels (sometimes excessively high, triggering migraines and heavy periods), the next you’re in a deficit. This matters for longevity because oestrogen is a master regulator of mitochondrial function. When oestrogen levels crash, your cellular power plants struggle to produce ATP efficiently, leading to the “brain fog” and fatigue that many women describe as feeling like their “lights have been dimmed.”
Beyond the “Average”: The 200 pmol/L Threshold
In conventional medicine, “normal” ranges for oestrogen are broad. In longevity medicine, we look for optimal ranges. Research suggests that the protective benefits of oestrogen for bone density, cognitive health, and cardiovascular integrity are strongest when blood levels remain above a minimum threshold—typically around 200–350 pmol/L.
If your levels are consistently below this, you aren’t just dealing with symptoms; you are potentially losing the “shield” that protects your arteries and brain tissue from age-related decline.
This distinction between ‘normal’ and ‘optimal’ is the core difference between conventional symptom management and a longevity-focused approach. In traditional practice, a woman whose levels fall within a broad laboratory reference range might be told she is ‘fine,’ even if she is still symptomatic and experiencing the subclinical loss of bone and cognitive protection. In contrast, longevity medicine is always aiming for a functional, protective level, seeking to replicate the conditions of a younger, healthier hormonal environment. This is a precision-led philosophy, moving away from average health to truly personalised healthspan.
The “Slow Burn” Hormones: DHEA and Testosterone
While oestrogen and progesterone are the “headline” hormones, DHEA and Testosterone play a massive role in your “healthspan.” These decline more gradually in perimenopause (similar to the male experience of andropause), but their loss is a primary driver of sarcopenia—the age-related loss of muscle mass.
Muscle is your metabolic currency. Losing it increases insulin resistance and reduces your physical resilience. Optimising these androgens isn’t just about libido; it’s about maintaining the engine that keeps you moving and metabolically healthy into your 80s and 90s.
Bioidentical (BHRT) vs. Synthetic: Why Structure Matters
There is a profound difference between a hormone that is “similar” and one that is “identical.”
Synthetic progestogens (often used in conventional HRT) have a chemical “tweak” that allows them to be patented, but this tweak means they don’t always fit the receptor perfectly. They can “spill over” into androgen or glucocorticoid receptors, leading to side effects like acne or bloating. Crucially, synthetic versions do not convert into the calming allopregnanolone in the brain.
Bioidentical hormones (BHRT)—or “Body Identical” when referring to licensed versions like micronized progesterone—are molecularly indistinguishable from what your ovaries once produced. They fit the receptors like a key in a lock, providing the benefits without the systemic “noise” of synthetic versions.
The Safety Renaissance: From WHI Fear to the 2025 FDA Milestone
For decades, a “black box” of fear hung over HRT, largely due to the misunderstood 2002 Women’s Health Initiative (WHI) study. In the UK, prescribing rates plummeted from 30% to just 14% almost overnight. We now know that study was significantly flawed, testing synthetic hormones on women who were often well past the menopausal transition.
The tide has finally turned. In a landmark move on November 10, 2025, the FDA officially removed the “black box” warnings for many HRT products, acknowledging that the risks had been overstated for younger women.
Here in the UK, this mirrors the long-standing efforts of the British Menopause Society to highlight the “window of opportunity.” For most women starting HRT within 10 years of menopause, the benefits for heart, bone, and brain health far outweigh the risks. At Agami, we use this window to front-load your health defences using only the safest bioidentical options.
The Longevity Mindset: Beyond Hormone Replacement
It is easy to focus on hormone replacement as the single solution to perimenopause, but at Agami, we see it as a critical piece of a much larger, multi-systemic puzzle. Bioidentical Hormone Replacement Therapy (BHRT) is the foundation that replaces the lost ‘shield’ of oestrogen and progesterone, helping to resolve debilitating symptoms like hot flushes, brain fog, and anxiety. However, replacing these hormones alone is not the finish line—it’s simply the starting line for true healthspan optimisation.
The decline in protective hormones accelerates the hallmarks of ageing across multiple tissues. To truly support healthier longevity and protect your future self, our strategy must move beyond simple replacement to proactively reinforce the core pillars of physical resilience that hormones influence:
- Muscle Mass & Metabolic Health: As the document highlights, the loss of DHEA and Testosterone directly contributes to sarcopenia, the loss of muscle mass. Muscle is the body’s primary metabolic organ, regulating blood sugar and insulin sensitivity. Our approach emphasises personalised nutrition and resistance training protocols to build and maintain this ‘metabolic currency,’ ensuring your cells remain responsive and energetic, countering the shift toward insulin resistance that often accompanies the hormonal transition.
- Skeletal Integrity & Bone Density: While oestrogen is essential for preventing the rapid bone loss seen in early menopause, bone health is a complex symphony involving Vitamin D, Vitamin K2, calcium, and mechanical loading. A strategy that does not combine BHRT with a targeted exercise regime (strength training) and bespoke micronutrient optimisation is incomplete. We aim not just to halt bone loss, but to actively drive bone strength.
- Body Composition & Visceral Fat: Hormonal shifts often trigger a relocation of fat storage, moving it from the hips and thighs to the abdomen as more metabolically-risky visceral fat. This is a critical driver of chronic disease. By measuring and actively improving body composition—reducing visceral fat and increasing lean muscle mass—we directly mitigate cardiovascular and metabolic risk, ensuring the ‘shield’ provided by BHRT is complemented by a resilient, healthy internal environment.
This holistic view acknowledges that perimenopause is a complex recalibration. Our goal is to leverage BHRT to restore balance, while simultaneously building robust, age-defying physical and metabolic foundations.
The Agami Approach: Precision, Not Guesswork
We don’t believe in “one size fits all” hormone dosing. Your skin absorbs patches differently than your neighbour’s; your liver metabolises pills differently than your sister’s.
Our functional medicine approach includes:
- Comprehensive Blood Panels: We track your levels against that 200 pmol/L threshold, not just “reference ranges.”
- DUTCH Testing: This “Dried Urine” test allows us to see how your body is metabolising hormones—ensuring they are breaking down into protective rather than inflammatory pathways.
- Baseline DEXA & Body Comp: We measure your bone density and muscle mass at the start, ensuring our interventions are actually moving the needle on your physical longevity.
Is BHRT Right for You?
Perimenopause is a transition, but it doesn’t have to be a crisis. While BHRT isn’t suitable for those with hormone-sensitive cancers or severe liver disease, for the vast majority of women, it is a safe, evidence-based tool to reclaim vitality.
The hormonal system is a symphony. When one instrument goes out of tune, the whole performance suffers. At Agami, our goal is to help you conduct that symphony with precision, ensuring your “second act” is your most vibrant yet.
Ready to redefine your transition? Book a Discovery Call Here.