The DNA of the microbiome in your body outnumbers your own DNA by a factor of 100 – it should therefore come as no surprise as to how many different functions these remarkable microorganisms serve for human health. I will take you through 5 important ways your microbiome can serve your health, as well as things you can do to help create a fertile soil in your gut for a rich diverse microbiome.
Keeping your bowel ticking over smoothly
It is thought that between 10-20% of people in the UK have IBS, and potentially even much more as many people do not seek medical help for their symptoms. Common symptoms of IBS include abdominal pain, bloating, diarrhoea, constipation and flatulence, amongst others. Dysbiosis (an imbalance of the microorganisms) of our gut microbiome has been shown to play a big part in initiating and fuelling symptoms of IBS1.
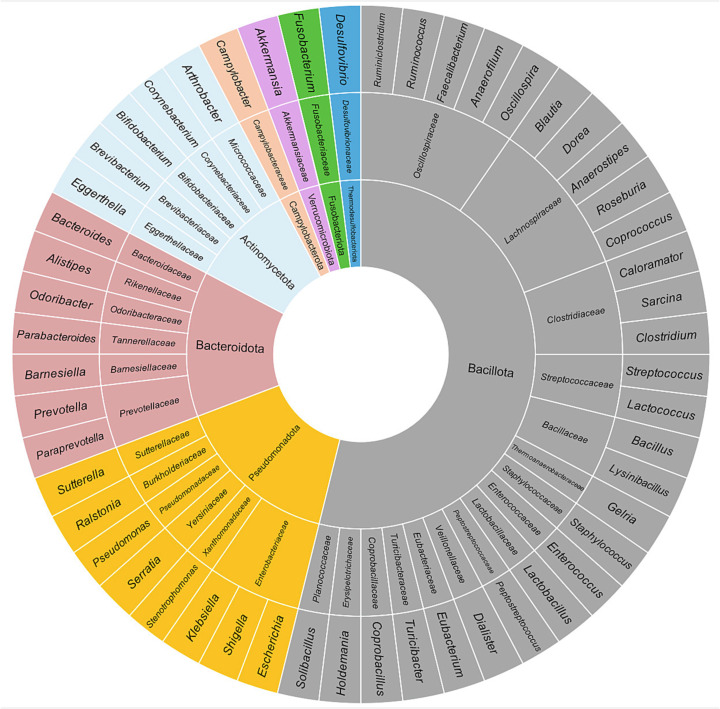
For example. certain microbiome patterns have been associated with IBS with constipation, including high levels of Bacteroidetes and lower levels of Actinobacteria (e.g. Bifidobacteria)2. It is thought that certain bacteria may attach to cells on the inside of your bowel and cause reduced motility of the bowel.
We should therefore pay attention to what lives in this ecosystem within our gut if we are to keep our gut ticking over smoothly.
Metabolic health
How our body absorbs and processes the food we eat plays an integral part in our health. In particular how we metabolise fats and carbohydrates (glucose in particular) plays a big role in major diseases like diabetes and heart disease. The microbiome has been shown to affect your risk of being overweight or obese. It does this in many ways, such as modulating digestion of macronutrients as well as regulating our hunger4.
When the healthy organisms in our gut breakdown fibre and nutrients in our diet, they release something called short chain fatty acids (SFCAs). These have been shown to trigger the release of a number of satiety hormones in the body – hormones that tell us we are full. One such hormone released is glucagon-like peptide 1 (GLP-1) – this is the same compound targeted by the latest craze of weight loss drugs being prescribed called GLP-1 agonists such as Ozempic and Trulicity.

These examples makes it easy to see how optimising your microbiome may help improve your metabolic health.
Keeping your immune system in check
Our gut is our biggest interface with the outside world (yes the inside of your gut is actually the outside world!). As a result, the gut is also where a large part of our immune system exists. There are a huge number of conditions that are due to an overactive immune or inflammatory response, something which can often originate in the gut. The immune system is all about balance between pro- and anti-inflammatory processes – you want an immune system that reacts appropriately to dangerous pathogens but does not overreact to harmless ones.
Having a healthy diverse gut microbiome can be thought of as a good education for your immune system. Coming into constant contact with the healthy microorganisms in the gut means the immune system learns how to tolerate and handle these, without triggering an exaggerated response of inflammation that then propagates through your whole body leaving you more prone to things like eczema, allergies and other inflammatory and auto-immune conditions.
Below is a figure from a study that showed the link between the ratio of Bacteroidetes and Firmicutes in the gut flora was linked to a change in the immune response, shifting from immune tolerance to inflammation and autoimmunity. Don’t get bogged down in the details of the different T cells (these are just different parts of the immune system which have slightly different functions). The important point this figure shows is the shift in immune response linked to the shift in microbial balance.

Cancer
While there are many factors that contribute to the unfortunate development of a tumour, the microbiome represents an important modifiable risk factor for many cancers. It is thought that dysbiosis contributes to 20% of all cancers5.
The large intestine has around 10 times the amount of bacteria compared to the small intestine6. It is therefore no coincidence that the incidence of cancer of the large intestine (colon) is 12 times higher than that of the small intestine8. There are a number of particular species of bacteria that have been associated with the development of colorectal cancer6.
Interestingly, the cancer risk from dysbiosis extends beyond the gut itself. The development of breast cancer is often (but not always) dependent on the hormone oestrogen which can promote tumour development. The liver normally gets rid of oestrogen from our bodies by combining it with something called glucuronic acid. The combined product is released into the gut and as it cannot be reabsorbed in this state, it is eliminated in our stools. Certain bacteria can exist in a state of dysbiosis which breaks the bond between the oestrogen and glucuronic acid, thus allowing it to be reabsorbed into the blood stream and increasing total body exposure to oestrogen in the long run8.
Mental Health
The gut is also known as the “second brain”. It contains around 500 million nerve cells which comprise what is called the enteric nervous system9. There is a very direct connection between the gut and your brain which works both ways. This connection is often referred to as the gut-brain axis. If we also include the microbiome, this is referred to as the microbiota-gut-brain axis. Below is a figure showing how the microbiome can affect the function of the brain both through a direct connection via the nervous system, but also via the immune and hormonal communication systems.

Given the above, it makes sense to make gut health an important part of holistic mental health care – with a big part of gut health being fostering a healthy microbiome. The inflammation also triggered by dysbiosis in the gut has its effects far and wide in the body, including the brain, thus playing a significant part in depression and anxiety, amongst other mental health disorders10.
So what can I do about it?
There are a few principles to try and keep our gut microbiome thriving and healthy. The biggest one being eating a diet high in colourful, fibre rich plants and whole foods, while minimising intake of processed foods. However, often the generic principles are not sufficient to achieve optimal balance as everyone’s imbalance can require specific treatments/tools to correct.
At Agami Health we are able to comprehensively test your gut microbiome and identify imbalances that may increase your risk of all of the above, and more. We are able to give you personalised treatment plans which include detailed nutrition plans, recommendations for pre- and probiotics and other treatments which are sometimes needed to restore optimal balance in your microbiome.
Contact us to find out how we can help you achieve the optimal balance in your microbiome and all the health benefits that come with this.
References
- Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018 Jul 9;7:F1000 Faculty Rev-1029. doi: 10.12688/f1000research.14592.1. PMID: 30026921; PMCID: PMC6039952. Link
- Ohkusa T, Koido S, Nishikawa Y, Sato N. Gut Microbiota and Chronic Constipation: A Review and Update. Front Med (Lausanne). 2019 Feb 12;6:19. doi: 10.3389/fmed.2019.00019. PMID: 30809523; PMCID: PMC6379309. Link
- Turnbaugh PJ et al. The human microbiome project. Nature 449, 804–810 (2007). Link
- Cox, T.O., Lundgren, P., Nath, K. et al. Metabolic control by the microbiome. Genome Med 14, 80 (2022). https://doi.org/10.1186/s13073-022-01092-0. Link
- Akbar, Noor & Khan, Naveed & Muhammad, Jibran & Siddiqui, Ruqaiyyah. (2022). The role of gut microbiome in cancer genesis and cancer prevention. Health Sciences Review. 2. 100010. 10.1016/j.hsr.2021.100010. Link
- Gagnière J, Raisch J, Veziant J, Barnich N, Bonnet R, Buc E, Bringer MA, Pezet D, Bonnet M. Gut microbiota imbalance and colorectal cancer. World J Gastroenterol 2016; 22(2): 501-518 [PMID: 26811603 DOI: 10.3748/wjg.v22.i2.501]. Link
- Proctor LM. The human microbiome project in 2011 and beyond. Cell host & microbe. 2011 Oct 20;10(4):287-91. Link
- Ruo SW, Alkayyali T, Win M, Tara A, Joseph C, Kannan A, Srivastava K, Ochuba O, Sandhu JK, Went TR, Sultan W, Kantamaneni K, Poudel S. Role of Gut Microbiota Dysbiosis in Breast Cancer and Novel Approaches in Prevention, Diagnosis, and Treatment. Cureus. 2021 Aug 26;13(8):e17472. doi: 10.7759/cureus.17472. PMID: 34513524; PMCID: PMC8405251. Link
- Fleming MA 2nd, Ehsan L, Moore SR, Levin DE. The Enteric Nervous System and Its Emerging Role as a Therapeutic Target. Gastroenterol Res Pract. 2020 Sep 8;2020:8024171. doi: 10.1155/2020/8024171. PMID: 32963521; PMCID: PMC7495222. Link
- Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, Fagundes CP, Malarkey WB, Laskowski B, Belury MA. Marital distress, depression, and a leaky gut: translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology. 2018 Dec 1;98:52-60. Link